Podcast: Play in new window | Download (Duration: 37:29 — 24.6MB)
Subscribe: RSS
In this episode, I have the pleasure of speaking with Lily Nichols, RDN. She’s known for challenging common guidelines when it comes to nutrition and dietetics. She analyzes the research and dedicates her time to truly understanding what it implies. Today, we’re talking specifically about the research around salt for babies and how much they can really handle.
I hear from clients all the time that are concerned about how to limit the salt intake for their baby. The current guidelines just seem so difficult to follow, and often unrealistic given how much salt can be found in common foods. We’ll be talking all about those guidelines, and why we feel there isn’t a need to stress about this as much as some may have you believe. We’ll talk about how your diet at home may influence how much you need to be concerned about salt for your baby, what the research really says when it comes to what harm may be caused by salt, and what this means for you when serving solids to your baby – hint-hint: you definitely do NOT have to stress as much about this as you may think!
As always, if you get value from this episode, please subscribe, rate and review it on Apple Podcasts. And share it with your friends who are also starting solids with their baby, let’s take a bit of stress off everyone’s shoulders!
Additional resources:
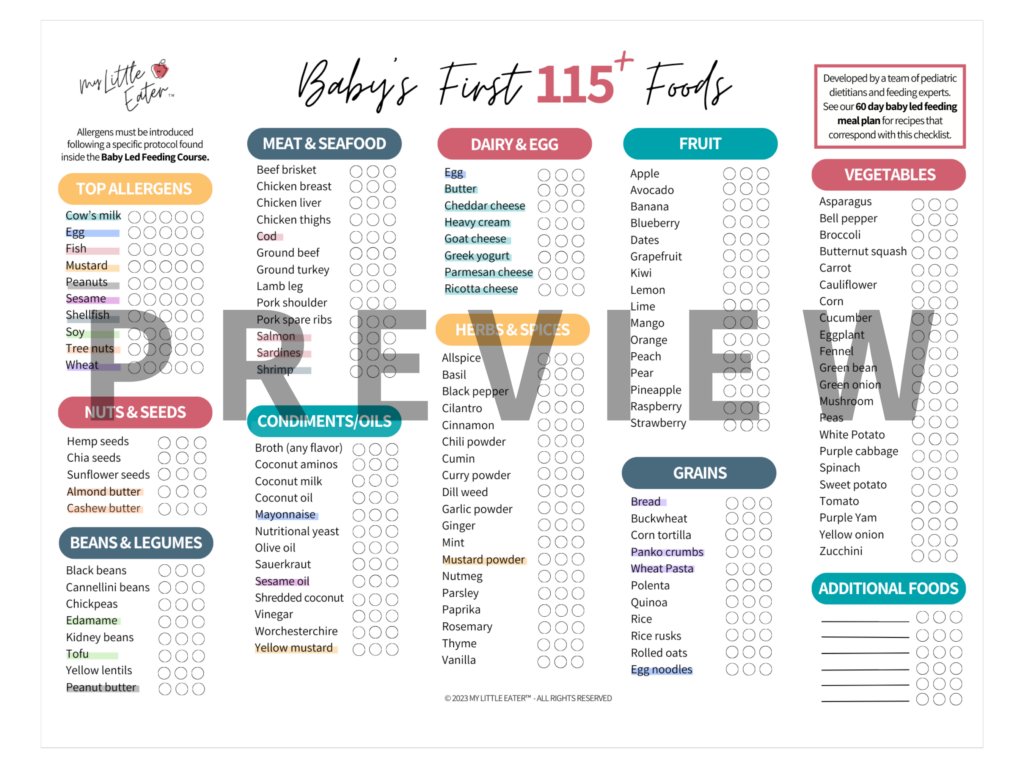
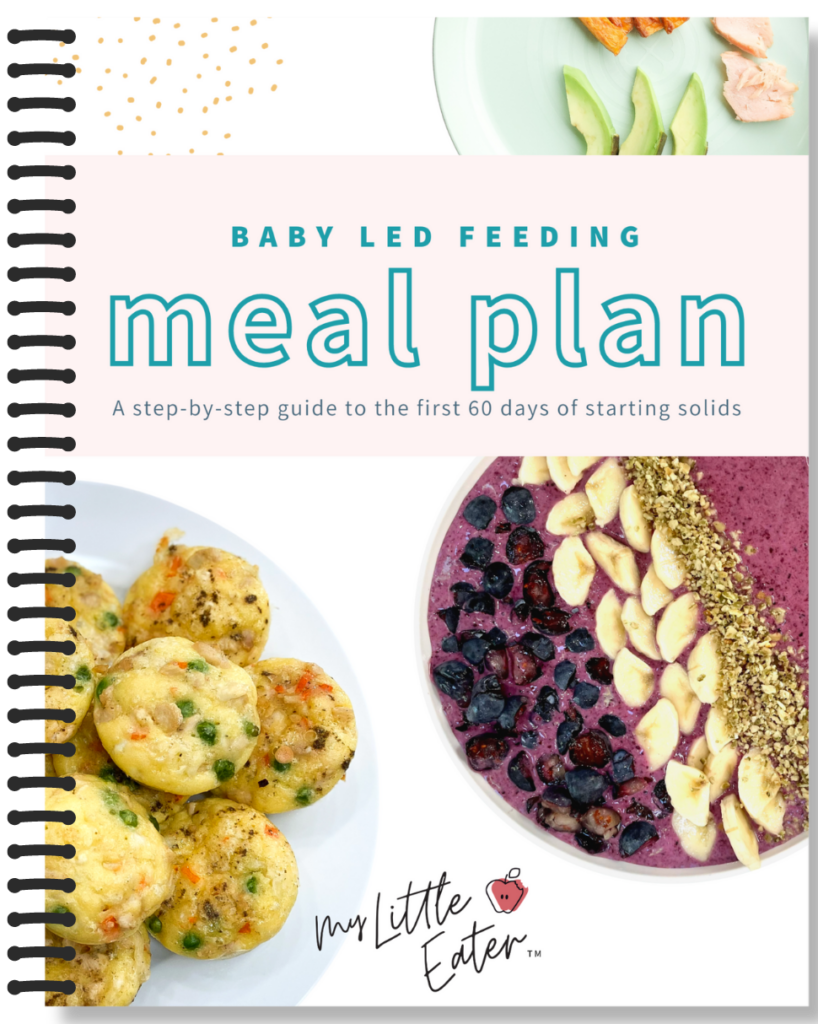
If you’re looking for my top recommendations on nutrition for your baby, and on safely serving all types of foods, introducing allergens, gagging vs. choking, and more – it’s time to enroll in my Baby Led Feeding online course! My new revamped version recently released, and it comes with the option to upgrade to include a 30 day meal plan where I show you exactly what to serve your baby (with over 60 recipes). (https://mylittleeater.com/baby-led-feeding/)
THE TRUTH ABOUT SALT FOR BABIES: https://mylittleeater.com/salt/
If you’re looking for more information on Lily Nichols’ work, you can follow her on Instagram, @lilynicholsrdn and also check out her post on salt for babies here: https://lilynicholsrdn.com/salt-baby-food-infant-sodium-requirements/
Lily’s Bio:

Lily Nichols is a Registered Dietitian/Nutritionist, Certified Diabetes Educator, researcher, and author with a passion for evidence-based prenatal nutrition. Her work is known for being research-focused, thorough, and unapologetically critical of outdated dietary guidelines. She is the author of two bestselling books, Real Food for Pregnancy and Real Food for Gestational Diabetes. You can find her work at LilyNicholsRDN.com
Skip to…
Welcome Lily! (0:52)
Myths regarding salt for adults (8:01)
Myths regarding salt for babies (13:25)
The official guidelines for salt intake for babies (21:54)
The main takeaway (35:12)