This blog has been contributed to by Ashley Cooley from @birth_baby_sleep. Ashley is a sleep expert and mom of 3! You can learn more about her and her work, here.
If your baby is in the 4 to 6 month age range, you’re probably wondering, will introducing solids affect how my baby sleeps? Some parents find their baby sleeps so much better after introducing solids, while others are complaining about their baby’s gas pains from solids that are keeping them up at night.
To be clear – if your baby was never sleeping well and you’ve started solids, well…the problem likely isn’t the solids and there’s work to be done on building good sleep habits instead.
However, if your baby was sleeping well and is now experiencing night wakings due to gas pains or tummy upset since introducing solids, you may need to consider making a few adjustments to the timing, quantity, and types of food being offered to baby (I’ll give you all the details below).

Table of Contents
Solids and sleep are very intertwined, and considering the fact that what you feed your baby and when you feed them has a big effect on digestion, it’s not hard to believe that they can affect one another! When first introducing foods, it’s a huge change to your baby’s digestive system, so knowing the best protocol for what to introduce, how to track symptoms, when to introduce food, and how to serve it to them is super important!
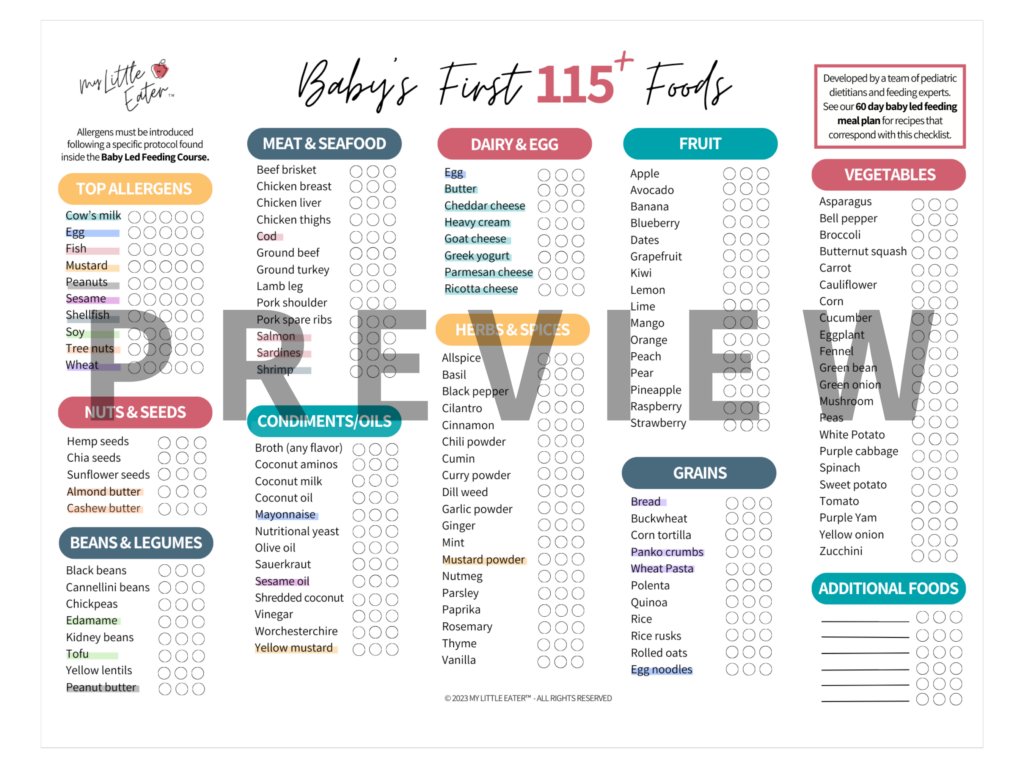
To find all the in-depth, research-backed info for feeding your baby all in one place, sign up for our Baby Led Feeding online course! Trusted by thousands of parents and experts worldwide, this course teaches you how to serve all foods safely using the feeding method that’s best for you and your baby, shows you how to progress through a variety of textures in a timely way with our signature Texture Timeline™ tool, and will have you confidently raising a healthy and happy eater!
At what age do babies no longer need breast milk or formula at night?
Before we dive into identifying if solids are affecting your baby’s night sleep, let’s make sure we’re clear on what to expect in regards to sleep around 6 months of age, which is around the time when your baby will be ready to start solids.

At 6 months, and all the way up until 12-14 months of age, babies will require about 15 hours of sleep within a 24-hour period (1). This means your little one should be sleeping approximately 11-12 hours throughout the night, plus 3 daytime naps with a total of 3-4 hours (1). At 6 months, babies do have the ability to stay asleep for 11-12 hours straight throughout the night, without waking for a nursing session or bottle feeding (1).
Babies don’t need milk at night from a nutritional perspective from around 6 months of age onwards.
If your baby is feeding at night (particularly if they’re doing so for long stretches of time, or for more than one feeding per night), this could be taking away from their appetite during the day. Consider removing, or significantly reducing, nighttime nursing or bottle feeding to regulate hunger cues and keep appetite open during daytime hours to avoid night wakings.
Will solid foods affect baby's sleep?

For most babies, starting solids doesn’t typically affect their quality of sleep.
And despite what someone may have told you, solids shouldn’t be used as a way to make babies sleep better, especially if they haven’t yet demonstrated all of the readiness signs for starting solids. There’s actually no research-based evidence to support that solids will help babies sleep better (this includes the myth about adding baby rice cereal to bottles). As a matter of fact, starting too early could do the opposite and make things worse instead of better. To learn more about why you shouldn’t start solids with your baby until closer to 6 months of age, check out our blog, here.
Could something else be causing new sleep struggles?

Your baby’s sleep struggles may not be caused by introducing solids at all! To determine what is causing your baby’s sleep struggles, ask yourself:
- Has baby always had poor sleep or regular night wakings?
- Have you noticed a difference in baby’s quality of sleep or sleeping patterns since starting solids?
- What are some other factors that may be impacting your baby’s sleep?
Your baby could be unsettled and waking overnight for a number of other reasons that aren’t related to food. If it happens at the same time that you’ve begun to introduce solids, it’s understandable that it may seem like the most obvious answer.
However, be mindful and rule out all other possibilities that could result in your baby having new or worsened sleep struggles. A change in baby’s normal routine due to changing nap schedules or awake windows, the onset of an illness, teething, or baby’s stage of development (ie. practicing new skills) could be the culprit.
If solids are causing your baby’s sleep struggles, let’s discuss what changes you can make to ensure your baby is getting a good night’s rest, while continuing to introduce solids and maintain adequate milk feedings throughout the day.
Reasons for struggling with sleep after starting solids
Starting solids made your baby’s reflux worse

Reflux is a common issue among babies and typically increases between 2 months and 6 months of age, likely due to an increased volume of liquid at each feeding, and then starts to decrease after 7 months of age. The good news is that reflux resolves in about 85% of infants by 12 months and in 95% by 18 months.
Being a digestive issue, introducing solids to your baby will likely have an impact on reflux symptoms. But depending on the severity of baby’s reflux, starting solids can actually help improve symptoms in most babies who have mild reflux. When solids are introduced, around 6 months old, your baby’s digestive system has had the time to mature, and reflux symptoms begin to improve.
The thing is… every baby is different, so while some babies have improved symptoms after starting solids, other babies may experience an increase in reflux symptoms. There are some common trigger foods that may be the culprit, so it will be a bit of trial and error to identify what works best for your little one.
MLE tips to solve reflux

There is no one size fits all approach to managing reflux in all babies, but there are some known trigger foods that tend to cause an increase in reflux symptoms, including (2):
- Onions
- Garlic
- Broccoli
- Citrus fruits (and juices)
- Tomato and tomato-based products
- Spicy foods
- Brussel sprouts
- Cabbage
- Cauliflower
- Corn
Offer common trigger foods in small amounts to start, and monitor their symptoms to determine if there’s a reaction. If there’s no reaction, you can continue to offer the food to baby. If baby does show signs of increased reflux symptoms, avoid offering the food for a few weeks, then reintroduce the food and monitor for symptoms again.
To further reduce the risk of reflux after feeding, baby should be kept in an upright, non-seated position for at least 20 to 30 minutes, a baby carrier or exersaucer may be helpful if you’re unable to hold baby upright for this length of time (sitting, as in an infant seat like a Bumbo, increases gastric pressure and is not helpful) (2). Therefore, you’ll want to avoid feeding baby right before they go down for a nap or before bedtime.
Starting solids is causing baby to wake up with gas pains or tummy upsets

Introducing solid foods to baby can be a little bit of a surprise to their digestive system. Up until this point, all their little bellies have ever known and digested was breastmilk or formula. So, it’s not unusual for babies just being introduced to solids to experience a bit of tummy upset, gas, more frequent bowel movements, or changes in the color and texture of their stool.
The type of food being introduced will have an impact on how your baby reacts. Certain foods cause more gas production, are a little bit more difficult to digest, or may cause changes in your baby’s stool. Now, you may be wondering if there are any foods you should avoid giving your baby to help prevent any tummy upset, so let’s talk about those now.
MLE tips to avoid the issue

- Offer solids in the morning versus later in the day or evening to avoid potential sleep disruptions throughout the night. By doing this, if baby does experience gas, it won’t be affecting them throughout the night when you’re trying to sleep too!
- Know the difference between gas that is painful and gas that is not. If baby seems to have increased gassiness since starting solid foods, but seems happy and playful without any signs of tummy pain, there is no reason to make changes to the food being offered. To help relieve baby’s gas, you can intervene by doing tummy massages and gentle exercises. Learn more about how to help your baby with gas, here.
- Identify which foods could be causing increased gas production. Certain foods will cause increased gas production but that doesn’t mean you have to completely avoid offering them to baby. You still want to provide them with exposure to all different types of food, so our suggestion is to only offer them in small amounts and avoid serving them at dinner time, in particular, to avoid sleep disruptions overnight. Plus, keep in mind that it may take some time for baby’s digestive system to adjust to certain new foods.
Foods that may cause increased gassiness include (3):
- Beans
- Broccoli
- Cauliflower
- Kale
- Artichokes
- Asparagus
- Brussels sprouts
- Cabbage
- Cauliflower
- Cucumbers
- Green peppers
- Onions
- Peas
- Radishes
- Apricots
- Bananas
- Melons
- Pears
- Prunes
- Peaches
- Raw apples
- Wheat bran
If you notice baby experiencing physical discomfort, tummy upset, vomiting, or is in physical pain after new foods are introduced, you could potentially be dealing with food allergies or sensitivities. In this case, you should avoid serving that food for the time being and contact your family doctor or pediatrician to determine the root cause of the issue.
Baby isn’t getting enough daytime calories

If infant sleep problems arise after starting solids, the first thing to do is evaluate the type of foods you’re offering baby and how much. When babies start solids at around 6 months old, and even up until 10/11 months, breastmilk or formula will provide them with all of the nutrients and calories they need. During this time, solid food is complementary to milk and shouldn’t be making up the bulk of your baby’s diet.
That being said, if baby is consuming lots of solids throughout the day that aren’t as calorically dense as breastmilk or formula, they may end up being unsatisfied and hungry throughout the night.
Breastmilk/formula is ounce for ounce much more nutrient dense than say – pear, banana, rice, or oatmeal. Many of the foods typically fed to babies, especially in the first few weeks of offering solids, are single-ingredient meals that aren’t completely balanced nutritionally, and lack enough healthy fat, protein, and carbohydrates. If your baby is food-loving and focuses on eating these types of foods in place of their regular amount of milk, then the result will be not enough caloric intake throughout the day. This can cause baby to wake from true hunger for a milk feed that provides more calories throughout the night. This can truly turn into a vicious cycle because if baby starts having too many night wakings because they need additional milk feedings, it can then impact daytime food consumption.
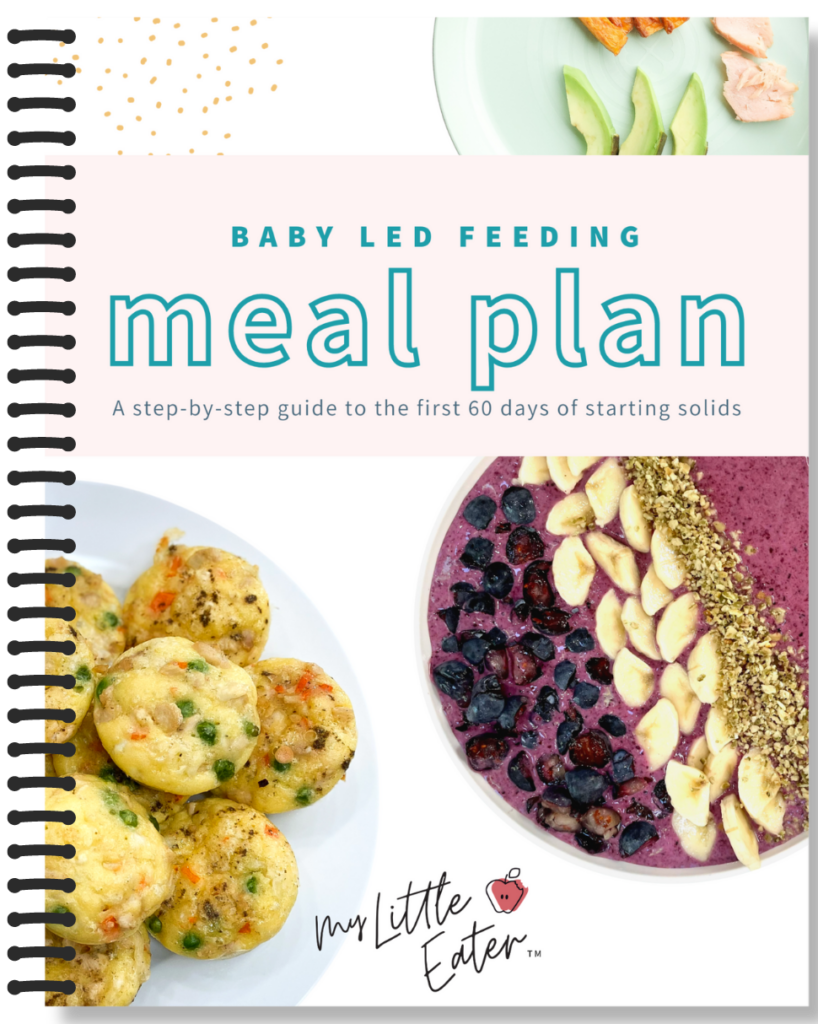
If you want to be sure your baby is getting nutritionally balanced and nutrient-dense meals, check out my 60 Day Baby Led Feeding Meal Plan – you’ll get access to over 80 recipes that are perfect for starting solids, and that the whole family can enjoy.
This isn’t just a regular meal plan with a list of recipes, you’ll actually be able to follow along with the plan to strategically introduce allergens, advance your baby in textures, and ensure all nutrient needs are being met.

MLE tip to ensure your baby is getting enough calories in
The best way to ensure your baby is getting an adequate number of milk feeds and getting their caloric needs met throughout the day is to stick to a feeding schedule, something flexible but predictable. Solids should be offered after a full milk feeding for the first few months at least, and there should be a minimum amount of milk they drink daily, based on their age.
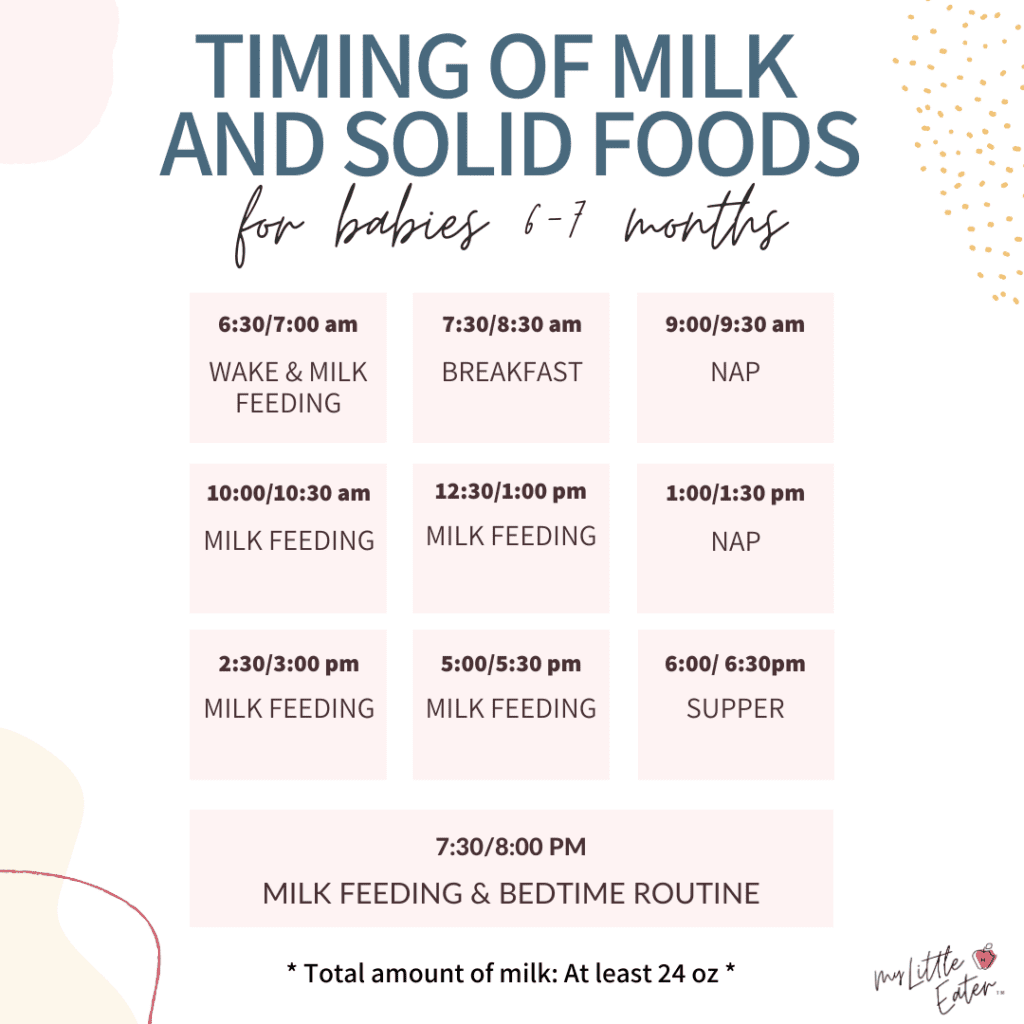
To learn more about feeding schedules and creating a daytime routine for your baby with sample schedules all the way up to 12 months old, check out our blog, here.
Baby is swallowing too much air
This may be a bit of a surprise, but chewing food properly is a very important part of digestion and it’s the very first step in the digestion process!

Chewing food thoroughly makes it easier for the stomach to process the food by breaking it down into much smaller pieces (4). When food isn’t chewed properly, it can cause digestive issues like increased gas production, constipation, and bloating (4). Chewing also increases saliva production, meaning it will make swallowing the food easier and safer for baby (4).
From a nutritional perspective, the more chewing and the smaller the food particles become, the easier it will be for baby’s body to absorb nutrients from that food (4).
MLE tip to help your baby learn to chew

Mouthing is the first step to control and advance chewing. Babies develop a simple up-and-down motion with their jaw between 5 to 9 months of age. They will then advance to diagonal jaw and circular jaw movements as time goes on.
A great place to start is giving your baby a variety of stick-shaped teethers to chew on daily. Once baby is ready to start solids, you can offer soft, stick-shaped foods and guide them to put the food between their molars. By placing it over the molar area of their mouth, baby will naturally learn to bite and chew. We also recommend modeling chewing to your baby during mealtimes in an exaggerated way (get silly with it too). You can say “chew, chew, chew” and then imitate big up and down chewing motions to baby with your mouth.
To learn more about teaching baby to chew, teaching baby how to take bites, mouth stuffing, and more, check out our blog, here.
Speak with a sleep consultant for further advice
Now that you’ve learned all of the tips to rule out food, caloric, and digestion-related issues causing sleep troubles for your baby, you can implement these strategies to determine the cause of your little one’s sleep struggles. If you aren’t seeing any improvement in your baby’s sleep after making these adjustments, it’s time to look for sleep-specific help and we’ve got you covered!
Ashley Cooley is the owner of Birth Baby Sleep. Their Bringing Up Baby membership is a hub for information about your baby when it comes to things like feeding, milestones, transitions, and of course, SLEEP! Members receive:
- Exclusive access to a ton of content
- Weekly, live virtual group sessions for education and connection
- Bringing Up Baby podcast recordings and Q&A with special guests
- A private community for connecting with others from wherever you are
- Unlimited access to a certified baby and sleep specialist

FAQs answered by sleep expert, Ashley Cooley:
The majority of 6 month olds are still napping 3 times per day, though it’s generally in the coming weeks that they’ll start the process of dropping down to 2 naps per day.
ABSOLUTELY. It’s still very common for babies to continue to wake for feeds well into their first year, but it might also be good to know that you usually can help to reduce night feedings by this time if they’re still waking a lot for them.
Usually, by 6 months of age, babies are either sleeping through the night entirely or are at least reduced to one overnight feeding. This is ok to do as long as they’re healthy/growing well and there are no concerns from baby’s doctor in doing so.
In fact, it can often help babies take in more solid foods as they grow if they start to eat less overnight.
The best way to help a baby fall asleep on their own in the middle of the night is to help them learn how to do it at the onset of sleep. It’s really hard to expect babies to know how to do it in the middle of the night, or that it’s even expected of them if we don’t show them how to do it when they’re first falling asleep.
This is what we call “sleep training” and there are a variety of ways to do it (aka it doesn’t necessarily mean “cry-it-out”). There are books on sleep training and an endless Google search that can help you figure out how to do it, but working with a sleep consultant generally helps families understand more about their particular baby and allows them to develop strategies that complement their approach to parenting – so it’s a more tailored approach.
Bedtime routines can vary from family to family, but having a process that takes less than about 20 minutes (after, or not including, bath time) is a good rule of thumb. Generally speaking, it might look something like this:
- Bath (*optional)
- Clean diaper & pajamas
- Breast milk or formula
- Brush teeth (*if present)
- Put on sleep sack
- Read a book, sing a lullaby, or cuddle
- Good night and lights out
A conducive sleep environment is one that provides comfort, is safe, familiar, and dark.
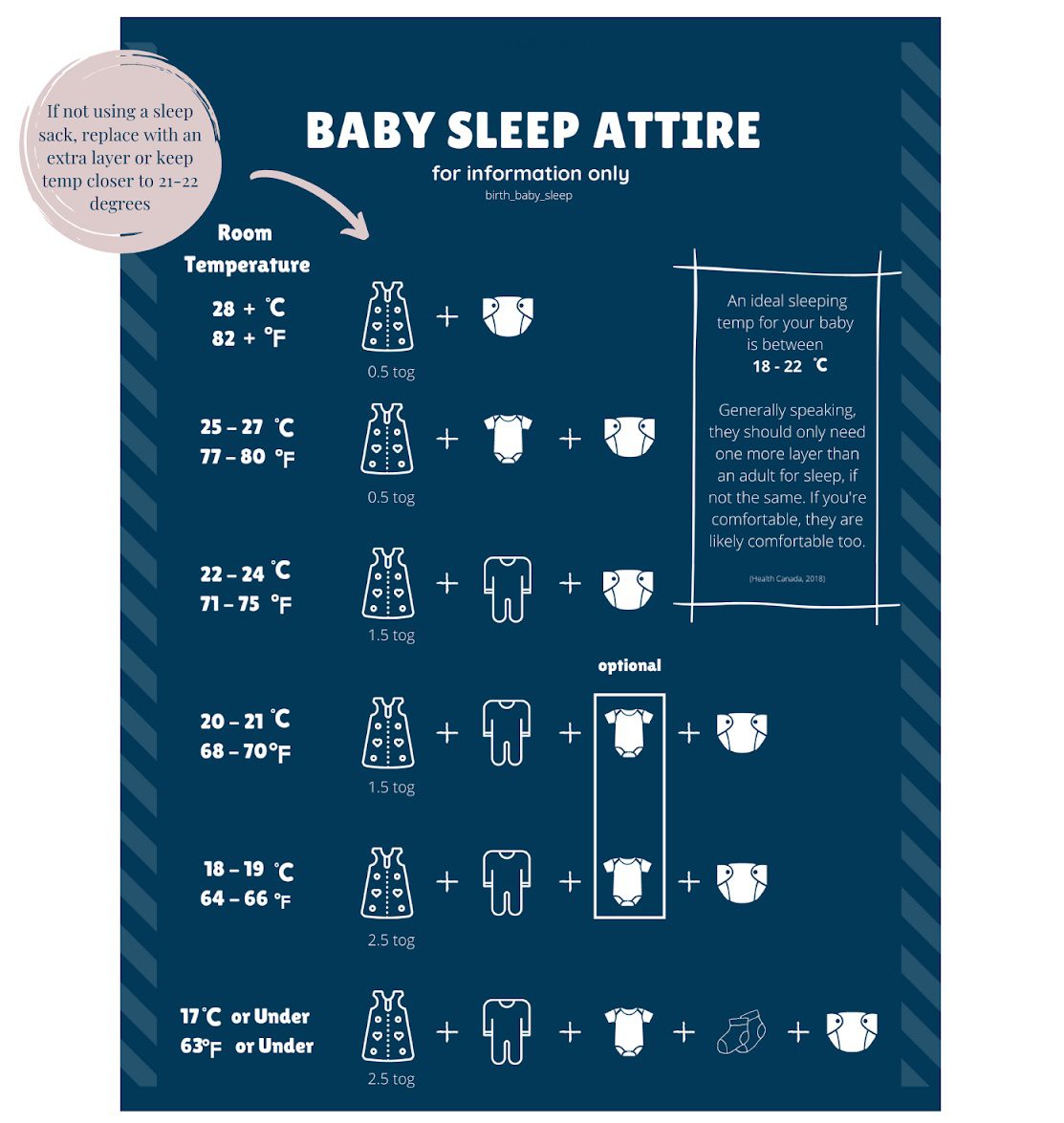
Comfort: Ideal sleeping temperatures are generally between 18-22 degrees Celcius (64 – 72 Fahrenheit), though not everyone has the luxury of controlling temperature in their homes so it’s most important that whatever baby is wearing is appropriate.
Safe: A firm mattress with a fitted sheet is all that’s in the crib/bassinet with your baby. A baby’s sleeping space should be free of loose blankets or clothing and away from hazards such as window blind cords.
Familiar: Helping your 6 month+ baby sleep in a regular sleeping space, like their room in a crib, is usually REALLY helpful for their sleep needs. Having familiar sounds, like a white noise machine, and wearing the same things, like a sleep sack, also bring familiarity and comfort for sleeping.
Dark: Blackout blinds aren’t usually a MUST-have, but the darker the room, the better! Darkness helps our bodies produce melatonin, which is the sleep hormone.
LOVE IT? PIN IT TO SAVE FOR LATER!
References:
- Little Z’s Sleep. Retrieved from https://littlezsleep.com/blog/5-month-old-sleep-schedule/; https://littlezsleep.com/blog/how-much-daytime-sleep-does-my-child-need/
- American College of Gastroenterology. Retrieved from https://gi.org/topics/gastroesophageal-reflux-in-children/
- International Foundation for Gastrointestinal Disorders. Retrieved from https://iffgd.org/gi-disorders/symptoms-causes/intestinal-gas/
- Patricia, J. J., & Dhamoon, A. S. Physiology, Digestion. 2019. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK544242/

ABOUT THE AUTHOR
CHELSEY LANDRY, RD
Community Dietitian at My Little Eater Inc., and bunny-mom to Hickory. Chelsey offers one-on-one counselling to parents of babies and toddlers that need more customized support. Learn more by booking a free discovery call with her today!

about the author
CHELSEY LANDRY, RD
Community Dietitian at My Little Eater Inc., and bunny-mom to Hickory. Chelsey offers one-on-one counselling to parents of babies and toddlers that need more customized support. Learn more by booking a free discovery call with her today!