Starting solids with your baby can be exciting, but we also know that introducing highly allergenic foods, like eggs, for the first time can feel TERRIFYING for many parents.
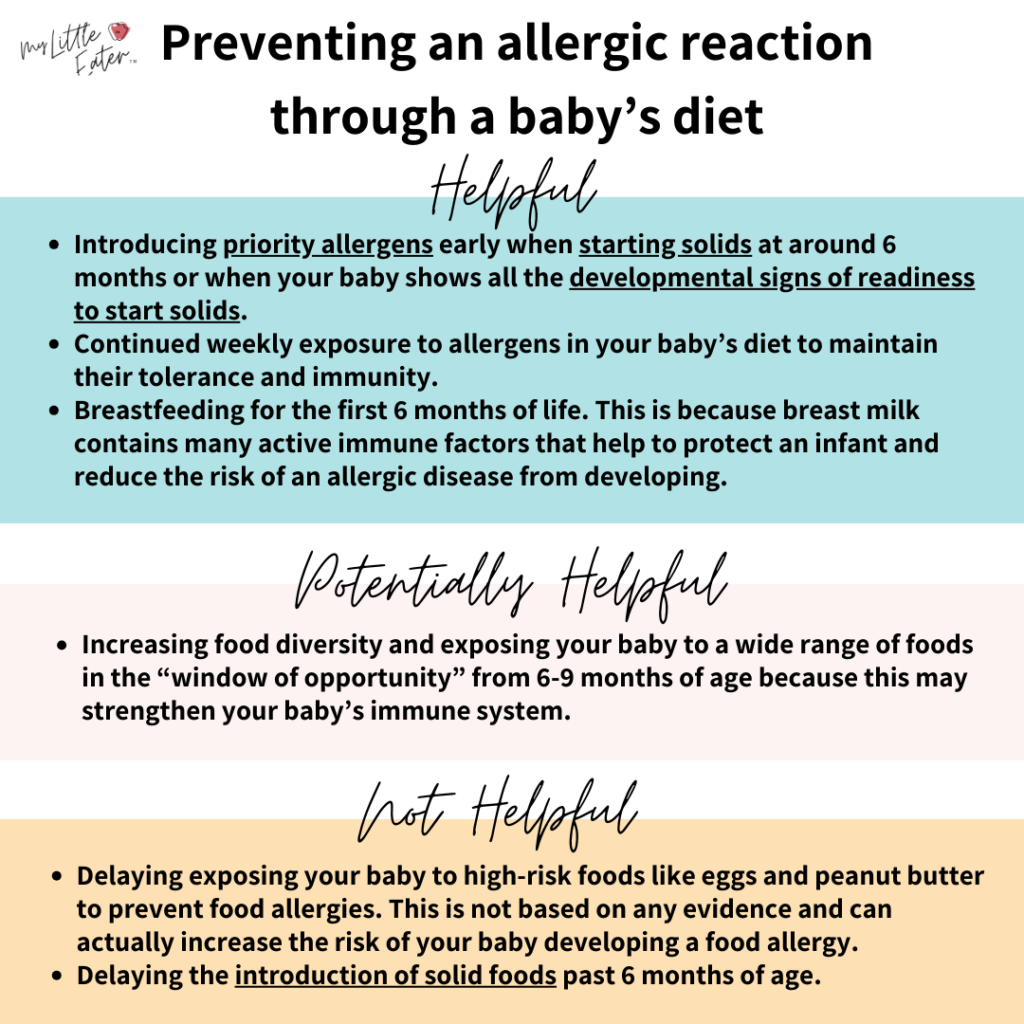
But did you know that timing is everything, and when you introduce priority allergens can actually reduce the risk of your baby developing an allergy?
We’ll tell you everything you need to know about eggs as an allergen, including what to do if an allergic reaction occurs so you can feel confident knowing that you’re prepared!
Table of Contents
Are eggs a common food allergen in babies?
It’s estimated that around 2% of children have an egg allergy, making eggs one of the most common allergens in babies and young children (1,2).
Luckily, around 70% of children with an egg allergy will grow out of it by the time they reach the age of 16 (1).

When to introduce eggs to babies
My Little Eater
Recommendation
Recommendation
When you introduce eggs to your baby is really important in reducing the risk of your baby developing an allergy.
Based on the latest research, we recommend introducing eggs to your baby early when starting solids, ideally between 6 and 9 months of age.
If you’re worried about your baby developing an egg allergy, you may be tempted to hold off on introducing eggs to them.
In fact, it used to be recommended to do exactly this and avoid introducing allergens like eggs until children were 1-3 years old. However, this was never based on any good research and was solely based on opinion (3).
The research has shown that early introduction of eggs is much more beneficial in developing an immune tolerance than delayed introduction (3,4,5).

Recent guidelines recommend that babies be introduced to eggs (and other allergens) around 6 months of age (and not before 4 months). They also recommend against delaying the introduction of allergenic foods to 12+ months (3,6).
Please note: solid foods such as eggs should not be offered before a baby is developmentally ready to start solids, which usually occurs around 6 months of age (6).
Furthermore, these new guidelines show the most benefit for high-risk babies. Infants at high risk for developing a food allergy include (3,6,7):
- Infants with eczema (moderate to severe are at the greatest risk).
- Infants with parents who have conditions such as asthma, eczema/atopic dermatitis, allergic rhinitis, or a known food allergy (8).
Impact of food diversity on allergies
There seems to be a “window of opportunity” in infancy between 6-9 months for creating a long-lasting immunity to allergens through food diversity.
Some preliminary research suggests that food diversity, or a greater variety of foods, can strengthen a baby’s immune system early on and may prevent food allergies from developing in both the short and long term (3).
Some research has shown that each additional food and priority allergen added to a baby’s diet between 6-12 months of age significantly lowers the odds of developing a food allergy and asthma in the first 10 years of life (6,9,10).
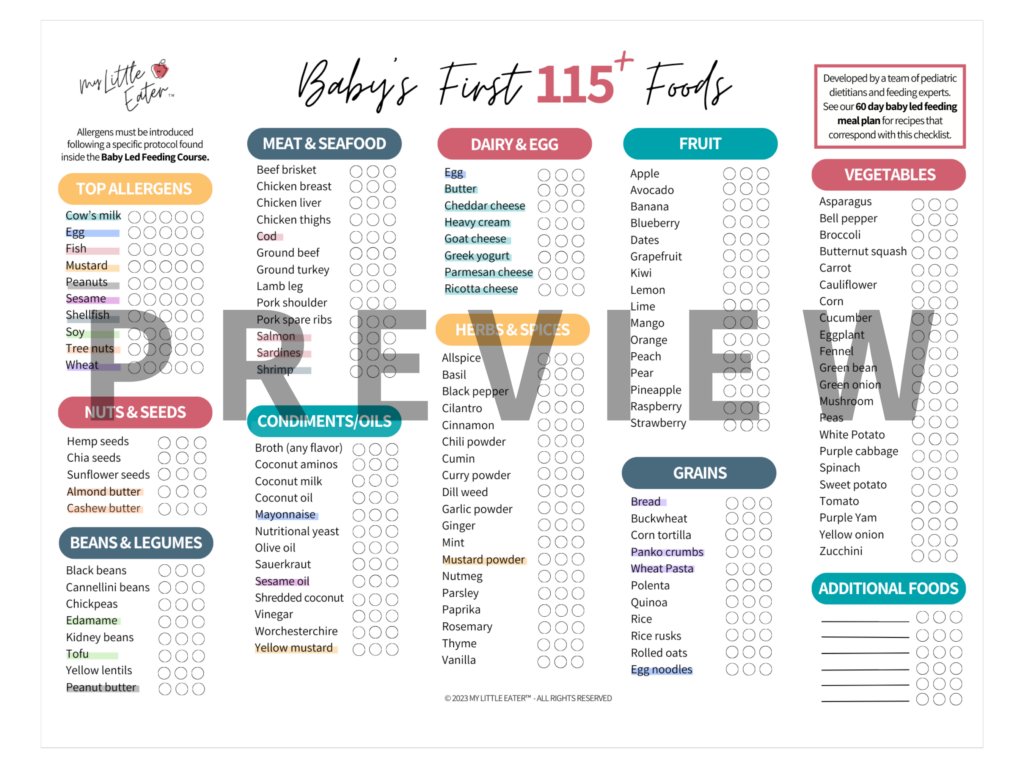
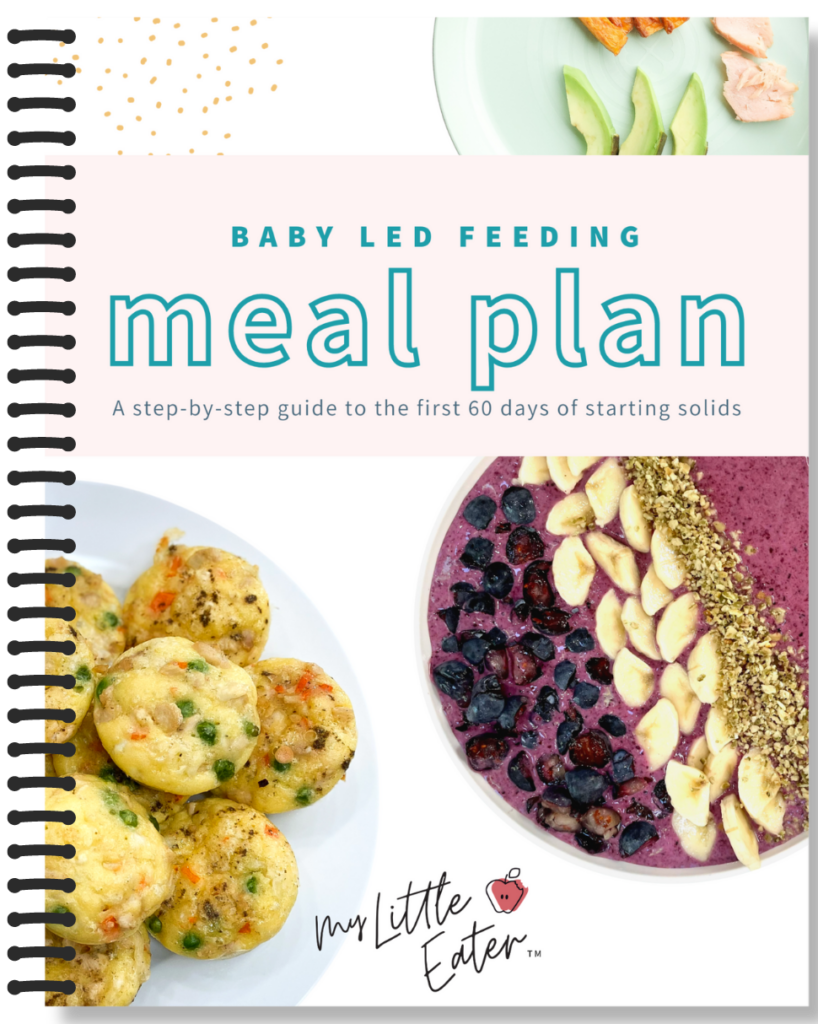
Check out our 60 day baby led feeding meal plan, which strategically introduces all of the priority allergens following the latest research.
The meal plan also introduces over 115 new foods in 9 weeks to help maximize the use of this critical period of 6-9 months to promote food diversity and set your baby up for success in life.
How to safely serve eggs to babies
Different types of eggs (i.e., scrambled, boiled, etc.) provide different texture experiences for your baby. However, all types of eggs (provided they’re fully cooked and modified appropriately) are safe for babies at around 6 months of age when your baby is showing all of the signs of readiness to start solids.
Some different types of eggs you can introduce to your baby are pureed, scrambled, boiled, as an omelet, or mashed and mixed with a binder like mayonnaise (AKA egg salad).

To find out how to safely serve all of these types of eggs to your baby, and to get a 5-minute egg in a mug recipe, check out our Texture Timeline™ egg resource.
5 tips to prepare for your baby’s first egg introduction
Knowing how to introduce an allergen and getting familiar with the signs of an allergic reaction before it happens can help you go into the experience more confidently.
Tip #1: Introduce eggs in isolation of other new allergens
When you serve highly allergenic foods to your baby for the first couple of times, you’ll want to be able to determine what your baby is reacting to if a reaction occurs. We do this by introducing eggs in isolation from other new allergens.
For example, don’t introduce eggs and soy in the same meal – if your baby reacts, you won’t know what they’re reacting to!
However, that doesn’t mean that you can’t serve other non-highly allergenic foods at the same time, such as bananas or broccoli. You can even serve top allergens that have already been ruled out as an allergy when introducing a new allergen.
For example, if introducing eggs for the first time by making an omelet for your baby, it’s ok to add cow’s milk when cooking, provided dairy has already been ruled out as an allergen. We just want to serve only one new priority allergen at a time so that we can properly monitor for reactions.
Tip #2: Serve eggs early in the day when your baby is healthy
The best strategy is to offer new allergens early in the day, for example at breakfast. This allows you to determine if an allergic reaction has occurred and gives you time to intervene if it does.

It’s important that your baby is healthy that day (no fever, runny nose, cough, etc.). We don’t want to have any allergy symptoms masked due to a previously existing illness.
We also recommend introducing new allergens, like eggs, in your own home, rather than allowing them to be introduced at daycare or when you’re dining out. This is so that you can ensure to follow the specific protocol for introducing allergens, and be able to monitor for reactions, seeking medical help if necessary.
Tip #3: Serve only well-cooked eggs
Eggs must be well-cooked when offering them to your baby or child.
There are different proteins in the egg white vs. the egg yolk that may trigger an allergic reaction, however, most people are allergic to the protein ovalbumin in egg white (11, 12,13). Ovalbumin is mostly broken down when heated thoroughly and is less likely to create an allergic response when fully cooked (12).
Serving slightly undercooked eggs to your baby could increase the chance of an allergy developing from the presence of more active allergenic proteins. Cooking eggs thoroughly may help reduce the risk of an allergy being triggered while creating a tolerance to the protein.
AKA – it’s a more gradual introduction to the allergy that improves tolerance and helps to prevent an allergy from developing later on.

From a non-allergy-related perspective, undercooked eggs can also contain the harmful bacteria Salmonella, which can cause foodborne illness in babies. With their immune systems still developing, babies are more at risk of severe complications from a foodborne illness and therefore cooking precautions such as this are crucial for their safety.
Tip #4: Know the signs of an allergic reaction
When you introduce eggs to your baby, watch for signs of an allergic reaction. To help, you can remove your baby’s clothing after the meal to monitor their body for reactions that may show up on their skin.
Allergic reactions usually aren’t severe the first time the allergenic food is eaten, but they should be taken seriously as a warning sign, as reactions can become much more severe with each exposure (14).
Common symptoms of a mild allergic reaction include any ONE of the following (15):
- Nasal congestion
- Sneezing
- Watery eyes
- Mild itchy skin
- Mild redness of the skin
- A few mild hives (not spreading, isolated to one small area)
- Mild gastrointestinal symptoms (such as a single episode of vomiting or diarrhea)

When mild symptoms become severe...
It’s important to know that even if symptoms begin as mild, they could evolve to be severe. If your baby begins to show more than one of the above symptoms, this could indicate the beginning of a more severe reaction.
This is especially concerning if your baby’s symptoms involve two or more different organ systems (16). For example, mild skin redness paired with vomiting (skin and gastrointestinal system) or mild hives paired with nasal congestion (skin and respiratory system).
In the case of multiple symptoms, call 911 and be sure to request that the paramedics bring an epinephrine auto-injector.
Common symptoms of a severe allergic reaction include (17):
- Widespread rash (redness, hives, or eczema)
- Swelling or itchiness of the lips and tongue
- Coughing or wheezing
- Difficulty breathing
- Change in skin or lip color (pale, blue)
- Continuous vomiting or diarrhea
- Blood in the stool
- Lethargy (your baby suddenly appears very tired, weak, or limp)
If your baby experiences one or more of the above symptoms, they may be at risk of going into anaphylactic shock.
Call 911 immediately and be sure to request that the paramedics bring an epinephrine auto-injector.
If your baby has an allergic reaction to eggs, you will usually begin to see symptoms within 10-20 minutes, with less severe reactions typically occurring within two hours after eating eggs (18,19).
If your child has a severe reaction, doctors now recommend continued evaluation because a delayed secondary reaction can occur, usually within 4-6 hours after the onset of the first reaction (20). This is why it’s important to introduce eggs early in the morning and seek medical help if a serious reaction occurs.
Check out our allergen guide for detailed instructions on introducing all top 10 allergens to your baby to help put your mind at ease!
Tip #5: Know how to respond to a reaction
Before offering eggs to your baby for the first time, you’ll want to be prepared in case they react.
If a mild to moderate reaction occurs that is not a medical emergency, you’ll want to have the number available for a nurse helpline, your doctor’s office, urgent clinic, or other medical services in your area.
This can help put your mind at ease and determine whether your baby needs to be seen immediately or if you can book an appointment for follow-up at a later date.

In the case of a severe reaction where medical attention is needed immediately, we recommend being prepared to call 911 (as discussed in more detail above). Do not attempt to take them to the hospital on your own, ask for an ambulance and advise them of the allergic reaction so they can come prepared with an epinephrine injector (EpiPen).
Though it may seem silly, check that your phone is fully charged and near you while introducing any allergens. If your baby has a severe reaction, especially if you’re concerned about possible anaphylaxis, this is the safest option.
Bonus Tips!
With all that in mind, we also recommend considering where you are and anything that may hinder your ability to have your child seen quickly. For example, if you live rurally and you know it takes an ambulance upwards of 20-45 minutes to respond to a call, it may be appropriate to introduce allergens at a friend or family’s house closer to a hospital – particularly if you’re very concerned or your baby is high-risk.
The same goes for introducing allergens while on vacation or out of the country. We recommend waiting until you’re home because emergency services may be more difficult to access or may incur additional fees when out of the country should a severe reaction occur.
For similar reasons, we wouldn’t recommend introducing allergens during any sort of inclement weather or emergency that may slow an emergency response down. For example, where we are in Canada, we often have snow storms and even hurricanes that make it difficult to travel on the road. Even if you’re home with your baby because of a storm, it’s likely not a great day to introduce a new allergen for the first time.

It certainly doesn’t hurt to be certified in first aid as well just in case of severe reactions. We recommend the Infant CPR Course by Safe Beginnings and you can use the code MYLITTLEEATER for 20% off.
Allergen protocol for introducing eggs to babies
There are two different options for how you can introduce eggs to your baby for the first time. Both are safe and effective ways of ruling out an allergy for your little one.
Choose whichever method below works best for you and your family!
Option 1: dive right in
Option 1 takes place over two days. It’s the standard method that we use in our 60-Day Baby Led Feeding Meal Plan.
Day 1
Step 1: Cook a whole egg until well done (the yolk should be firm, not runny). You may choose to cook the egg scrambled, hard-boiled, or as an omelet.
Recommended next...
Check out our Texture Timeline™ egg resource to learn how to cook and serve different types of eggs for your baby.
Step 2: Mash the cooked egg using the back of a fork, then serve a small amount (about ¼ tsp) to your baby.
Step 3: Monitor your baby closely for signs of an allergic reaction for the next 10 minutes. You can let your baby eat non-allergen-containing food while you wait.
Step 4: After 10 minutes are over, as long as they do not show any signs of an allergic reaction, offer your baby the rest of the egg alongside their regular meal. Just make sure that the meal doesn’t include any other new allergenic foods.
Step 5: Continue to monitor your baby for signs of an allergic reaction after the meal has ended (most symptoms of an allergic reaction appear within 2 hours after consumption).
Day 2
If your baby does not have an allergic reaction to eggs on day one, it’s important to serve them another egg-containing meal again on day two. Aim to serve at least 2 tsp of egg.
Again, be sure to monitor your baby closely for signs of an allergic reaction after the meal has ended (most symptoms of an allergic reaction appear within 2 hours after consumption).
If your baby does not have an allergic reaction on days 1 or 2, you can rule out egg as an allergy!

Day 3
This final step is optional.
Reintroduce the allergen for a third day to ensure enough egg has been consumed. With babies, it’s hard to know exactly how much they’ve eaten, so this third introduction is for reassurance that they got a true exposure to the allergen.
Option 2: ease into it
If you’re looking to introduce your baby to eggs more gradually, you can use this introduction method, which takes place over four days instead of two.
Step 1: Introduce 1/4 tsp of cooked, mashed egg alongside your baby’s regular meal. Just make sure that the meal doesn’t contain any other new allergenic foods.
Step 2: Monitor your baby for signs of an allergic reaction (most symptoms appear within 2 hours).
Step 3: If your baby does not have an allergic reaction, serve cooked, mashed egg to your baby again the next day in a slightly larger amount. Follow the table below for guidance on how much to offer each day.
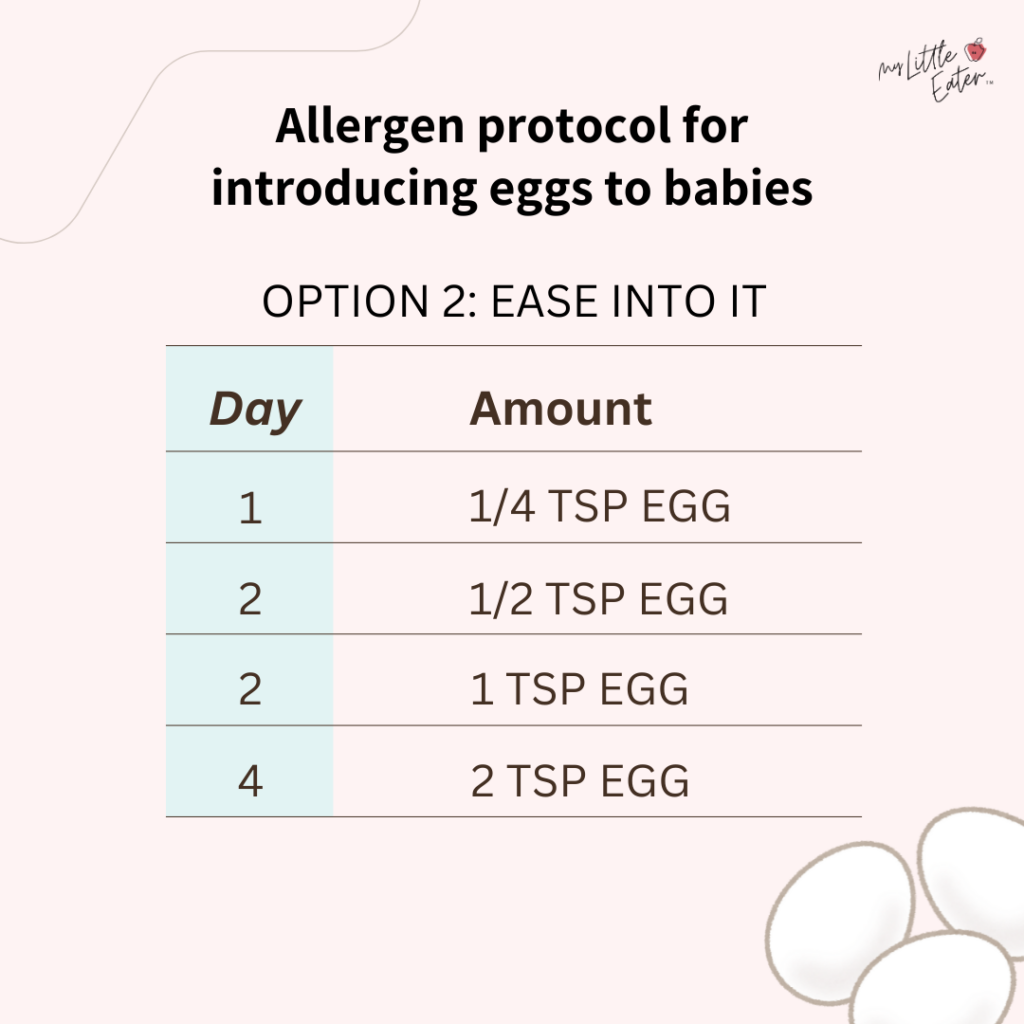
If your baby does not have an allergic reaction on days 1, 2, 3, or 4, you can rule out eggs as an allergy!
What to do if a reaction does occur
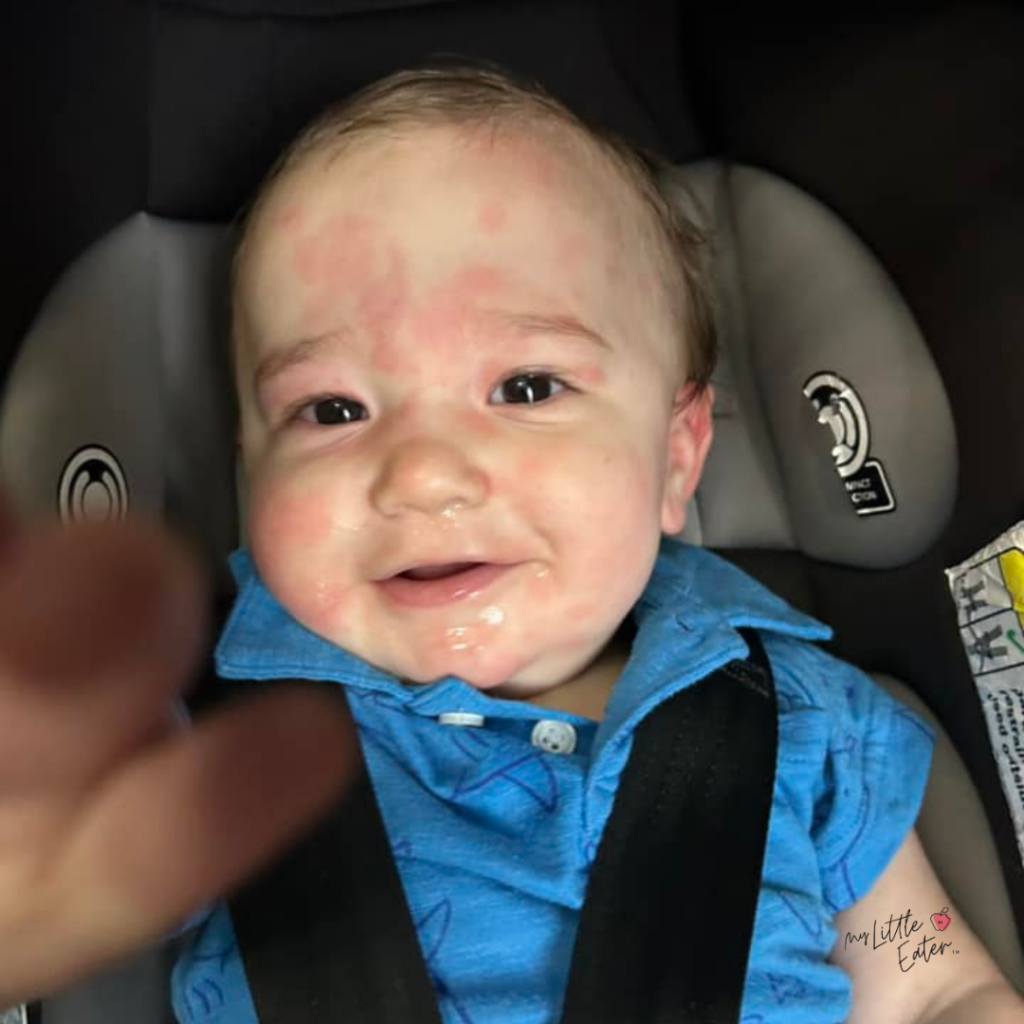
If you start to notice any symptoms, such as red appearing on the face, hands, or arms, you’ll want to check the rest of the body for other signs and symptoms right away.
Strip your baby down to easily observe all parts of their body, monitoring for signs that may appear, such as any redness or a rash spreading throughout the body.

We recommend taking photos of your baby’s symptoms and journaling the food they’ve eaten that day. This will be helpful for your baby’s doctor or allergist when they do their assessment.
If your baby is having a severe allergic reaction, such as anaphylaxis, call 911 and seek medical attention immediately.
As a reminder, your baby may be at risk for anaphylaxis if they are experiencing two or more signs of a mild allergic reaction, or one or more signs of a severe allergic reaction.
A sign of anaphylaxis may not only be wheezing and difficulty breathing, as many of us associate it with. Signs that may indicate a severe reaction and that anaphylaxis could still occur include a widespread, severe rash, lethargy, or continuous vomiting.
Can babies have Benadryl?
A recommendation we hear frequently is to have Benadryl on hand to treat symptoms. This is no longer recommended due to the side effects of Benadryl in babies.
As always, speak with your doctor before offering any medications to your child.
How long will symptoms last?
This can vary depending on the severity of the reaction, the amount of food ingested, and the immune system.

Milder reactions to food may only last a few minutes to hours. Skin irritations like hives typically resolve in less than 6 hours (19). More serious reactions could take days to subside, however, this is less common (21).
Recognizing symptoms of other types of reactions
FPIES
Eggs are a common trigger for Food Protein-Induced Enterocolitis Syndrome (FPIES) which is a type of non-IgE-mediated food allergy (meaning the reaction in the immune system doesn’t involve antibodies like with a regular allergenic response).
FPIES usually occurs in early childhood, and luckily, most children outgrow FPIES by 3 years of age (22,23).
Symptoms of FPIES are confined to the gastrointestinal system and include vomiting and diarrhea that manifest typically within 1 to 4 hours after eating the “trigger” food, like egg (22,24,25). Profuse, projectile vomiting may occur first followed by diarrhea (26).
Treatment for FPIES is avoidance of eggs in the diet and to ensure adequate hydration (22).
Mild symptoms and vomiting may resolve on their own within hours after a reaction occurs, once removing eggs from the diet (22,26). However, in some cases, medications may be needed to stop vomiting (26).
Additionally, dehydration can be a serious complication of FPIES.
Around 20% of children who experience a FPIES episode become severely dehydrated, resulting in the child becoming limp, cold, and pale (in shock) (26).
If your child is experiencing severe vomiting, diarrhea, dehydration, lethargy, pallor, or changes in body temperature, seek medical help immediately. In these severe cases of FPIES, rehydration through intravenous fluids is required (24,27).
The difference between FPIES and an allergy involving antibodies is…
- FPIES: Symptoms include vomiting and diarrhea and occur 1-4 hours after the trigger food is eaten.
- Allergy: Symptoms (as well as vomiting and diarrhea) may also include hives, swelling, and wheezing, and often occur within 15 minutes after eating the trigger food, and no later than 2 hours after.
If you suspect your child has FPIES, call your baby’s doctor or allergist and avoid serving eggs to your baby until you can meet with a specialist.
Contact dermatitis
Another type of food sensitivity is contact dermatitis, which can cause babies to develop a mild, temporary rash after eating acidic foods like tomatoes, pineapple, oranges, and strawberries – eggs are not typically triggers for this type of reaction, but anything is possible.
This type of rash appears around the mouth, hands, or wherever the food comes into contact with the skin only (28).
Contact dermatitis is harmless and should not cause any other symptoms of an allergy, such as widespread hives on the body (28). You can expect the rash from contact dermatitis to go away within approximately 30 minutes and even more quickly if you gently clean the affected area with a cold, wet cloth (29).
No follow-up with an allergist is typically required, and avoiding the food is not usually recommended, but please speak with your doctor if you do have concerns.
Eczema
Eczema is an inflammatory skin condition which causes red, scaly rashes. The rashes can occur anywhere on the body, cause itchiness, and are sometimes painful (30,31). Rashes can be brought on by various foods and items in your baby’s environment, such as soaps.
Atopic dermatitis is the most common form of eczema, especially in babies and young children (32).
Symptoms of eczema most commonly appear in babies before age 1, and luckily, most children will outgrow it (23). Nonetheless, eczema interferes with the skin’s natural protective barrier, making affected babies more vulnerable to developing an allergy (23,30).
It’s important to know the difference between eczema and an allergic reaction. Symptoms of an allergic reaction will happen quickly each time the “problem” food is consumed. Symptoms usually go away several hours after the food is eaten (32). Once the food is removed from the diet, the symptoms will resolve.
During an allergic reaction, symptoms such as hives, redness, and itching may be widespread throughout the body in unpredictable locations (32). An allergic reaction may also cause symptoms that eczema will not cause, such as potential swelling, vomiting, diarrhea, coughing or wheezing, etc. (33).
Eczema is chronic and does not go away quickly (32). While eczema can show up anywhere on the body, it sometimes shows up in predictable places, such as the cheeks, scalp, forehead, elbows, knees, or elbow and knee creases (32,33).
The rashes that come with eczema are also quite different from the raised hives that a food allergy can cause (33).


Raised hive from an allergic reaction
Red, scaly rash from eczema
If you’re unsure, make an appointment with your baby’s doctor. It can also help to keep a journal of all foods your baby has eaten prior to developing symptoms, and note their surroundings, such as soaps or creams recently used, what material clothing they had on, etc. (33). This may help rule out foods as triggers or their surroundings as contributing to an eczema flare-up.
What to do next if no reaction occurs
Once you’ve introduced eggs to your baby multiple times, following our allergen protocol, with no reaction, you can rule out eggs as an allergen. However, research suggests that continual ingestion of 2g per week (about ½ teaspoon) of egg is effective in preventing an egg allergy from developing.
We want to keep priority allergens showing up in the diet regularly to keep up your baby’s tolerance and immunity to the allergen proteins.
You can keep egg on the menu by serving foods like:
- Cheesy scrambled eggs
- Vegetable egg omelet
- Egg muffins or cups
- Shakshuka
- Fish or vegetable fritters (that include egg as a binding ingredient)
- Pancakes (that include egg as an ingredient)
- French toast
- Egg noodles
Check out our 60-Day Baby Led Feeding Meal Plan for recipes and for more ideas on how to include eggs in your baby’s diet!
How to move forward with an egg allergy
As you wait for your first appointment with your baby’s doctor or allergist, avoid serving eggs to your baby. However, there’s no need to stop offering other new allergenic food in the meantime, as we treat each priority allergen independently.

If your baby reacted earlier in the day, you don’t have to avoid feeding them for the rest of the day – even if they still have a rash or hives present. You can go ahead and feed them any non-allergenic foods or allergenic foods that you have already ruled out.
However, be sure to allow symptoms to clear up completely before offering any new priority allergens for the first time so that you can monitor for new symptoms.
The next time your baby is ready for a meal, as long as they’re feeling okay, you can get them back into the high chair and you can return to their schedule as usual.
Do you have to avoid eggs if you breastfeed?
If your baby has an egg allergy, they may react to egg proteins passed through your breast milk after you’ve eaten eggs (18,34).
We recommend that breastfeeding moms avoid eggs in the diet until you’ve seen your baby’s doctor or allergist for further guidance.
How to overcome your fear after an allergic reaction
If your baby has an allergic reaction – especially a moderate to severe reaction – it can be scary for you when your baby starts eating again. Particularly when introducing new foods!
Slowly easing back into things can be helpful.
Don’t feel like you need to dive into introducing new priority allergens to your baby. Give yourself some grace and take a little breather.
Focus on the smaller things, like getting back into a routine. Your little one may even feel a bit cautious about the highchair after the previous experience they had.
Focus on making mealtimes in the highchair exciting and even silly if you need to, and don’t worry too much about their intake for the time being. Let them play with food and get food on their hands. Play some light music and keep things upbeat.

It can help to remember that even though your baby had an allergic reaction and you may be terrified of it happening again…you’ve done it before, you made it through, and your little one is OK!
Treatment for an egg allergy
If your baby has an allergic reaction to eggs, you’ll need to avoid serving eggs or any egg-containing foods to your baby.
Since eggs are one of the allergens that children can grow out of, your baby’s pediatrician or allergist may suggest working through the “egg ladder” (35).
The egg ladder is a method used to build up a tolerance to eggs through very slow, gradual, and consistent exposures (36).
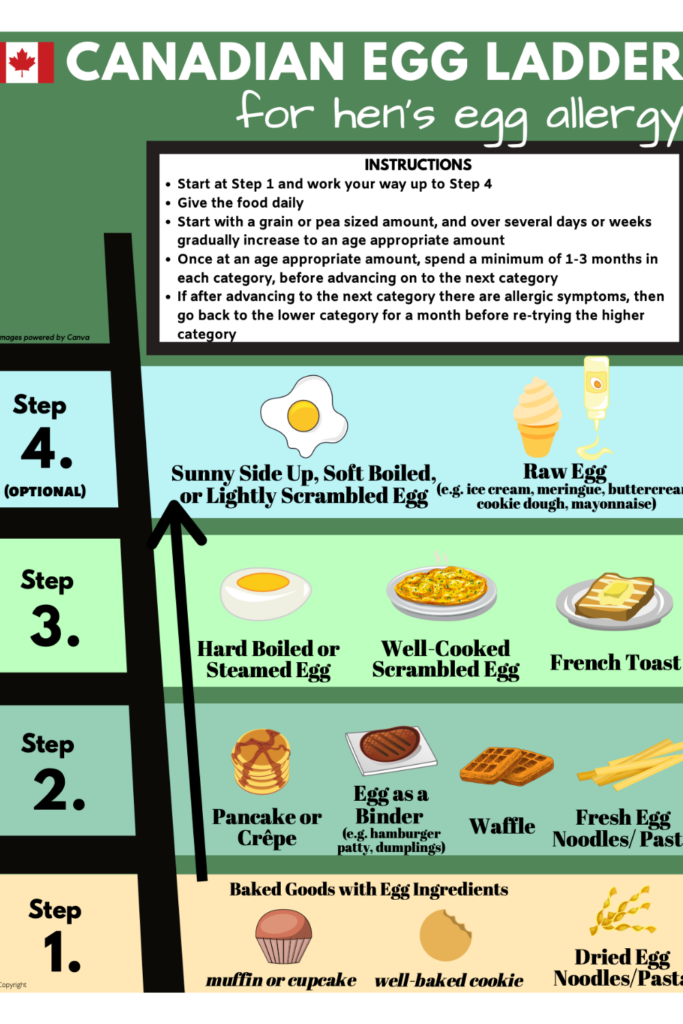
The first step consists of introducing a small amount of egg in a baked form, where only a little bit of egg is in the ingredient list. An example of this would be a muffin, where only one egg is divided between 12 muffins.
As the steps go on, larger quantities of eggs are introduced in less cooked forms until eventually your baby can tolerate eating eggs on their own or as part of a meal.
The egg ladder may not be recommended for every baby with an egg allergy, and not every baby with an egg allergy who goes through the egg ladder will be able to progress all the way to tolerating food items in step 4 (i.e., sunny side up, soft boiled, lightly scrambled eggs, or raw eggs in recipes).
Please do not follow the egg ladder unless you’re advised to do so by your baby’s pediatrician or allergist. Regular follow-ups with an allergy specialist and/or a Registered Dietitian are also recommended for babies who are working through the egg ladder (36).
Food products that may contain egg
If your baby is diagnosed with an egg allergy, you’ll have to be more cautious when buying and serving food to your baby. Many food products sold in the grocery store can contain eggs as an ingredient – and not all of them are obvious – so you’ll need to get into the habit of reading food labels.

If the package does not include a label, don’t buy it. Ingredients you may see on labels that indicate there is egg in the product are: egg, fresh eggs, dried egg powder, powdered eggs, yolk, egg substitutes such as Egg Beaters™, eggnog, globulin, livetin, lysozyme, meringue, and any word with ovo or albumen/albumin in it, such as ovoglobulin and ovalbumin (37,38).
Food products that commonly contain eggs as an ingredient (37,38):
- Baby food
- Baked goods and baking mixes
- Battered/fried foods
- Candy, chocolate
- Cream-filled pies
- Creamy dressings, salad dressings, spreads
- Desserts
- Egg/fat substitutes
- Fish mixtures
- Icing and glazes
- Meat mixtures (e.g. hamburgers, hot dogs, meatballs, meatloaf)
- Pasta
- Quiche, soufflé
- Sauces such as Béarnaise, Hollandaise, Newburg
- Soups, broths, bouillons
Egg substitutes for babies with an allergy
Nutritional substitutes
Nutritionally speaking, eggs are a convenient source of protein, vitamin B12, zinc, and more, making them an important addition to the diet for contributing to your baby’s overall growth and brain development.
Learn more about the nutritional benefits of eggs for your baby in our Texture Timeline™ resource on eggs.
If your little one can’t have eggs, it’s important to make sure that they’re getting these nutrients from other sources of protein in their diet.
Egg-free sources of protein include:
- Poultry (chicken, turkey)
- Meat (beef, pork, lamb)
- Fish (salmon, sardines, canned light tuna)
- Shellfish (shrimp, scallops)
- Tofu
- Legumes (beans, lentils)
- Dairy products (yogurt, cheese)
For more information or guidance on providing your baby with enough protein, vitamin B12, and zinc, speak to a Registered Dietitian.
Recipe substitutes
If you discover that your baby does have an allergy to eggs, you may find yourself looking for suitable alternatives when it comes to baking for your little one. Thankfully, there are quite a few different ways that you can substitute an egg in a recipe.
A note about egg substitutes
Some egg substitutes contain other common allergens such as milk, peanuts, and soy. Be careful to only introduce these substitutes to your baby after having ruled out these foods as allergens.
Stand-alone egg replacements
Tofu – Silken tofu and soft tofu mimic eggs in frittatas and quiches, while firm tofu or extra firm tofu work better for egg salad and scrambled eggs. Bonus – you can also use silken tofu or soft tofu to bind custard, egg sauces like mayonnaise, and pudding with a creamy, smooth mouthfeel!
“Just egg” egg replacement – If you need a ready-made liquid egg mixture that works well for making omelets or scrambled eggs, you can use this product that’s made from mung beans. It is a bit higher in sodium, so use this substitute in moderation.

Chickpea flour – When mixed with water, chickpea flour can mimic eggs in recipes such as omelets, frittatas, and quiches. It’s also high in fiber and contains important nutrients like iron, zinc, magnesium, and folate. You can mix in spices like onion powder, garlic powder, turmeric, etc. to make a delicious recipe!
Replacements for eggs in baked goods
Aquafaba – This is the liquid left over from cooking chickpeas (you can use canned or freshly cooked chickpeas). Just substitute 3 tbsp of aquafaba for one egg to use as a leavener, which helps things like muffins, pancakes, and cakes rise.
Carbonated water – This one may surprise you, but carbonated water can be used as a leavening agent for baked goods like cakes, crepes, muffins, pancakes, and waffles. Just use 1/4 cup of carbonated water as a replacement for 1 egg in a recipe.
Mashed, ripe banana or applesauce – While these will impart a sweet flavor, mashed banana or applesauce work great in many baked goods. Use 1/4 cup of ripe banana purée or applesauce as a replacement for 1 egg.
Note: Banana or applesauce won’t help baked goods rise, so this replacement works best in recipes that also include baking soda or baking powder.
Yogurt – Use 1/4 cup of full-fat yogurt as a substitute for 1 egg in recipes. This swap also doesn’t replace a leavening agent, so it’s best used in recipes that include baking soda or baking powder.
Egg replacements to use as a binder (for things like fritters, fish cakes, meatballs, or burgers)
Chia egg: Mix 1 tbsp of ground chia seeds with 3 tbsp of warm water, then let the mixture sit for at least 15 minutes in the fridge to thicken.
Flax egg: Mix 1 tbsp of ground flax seeds with 3 tbsp of warm water, then let the mixture sit for at least 15 minutes in the fridge to thicken.
Chia and flax eggs can also be used in baking as long as the recipe contains a leavening agent such as baking powder or baking soda.
FAQs
Can egg allergies be outgrown or desensitized?
Yes. While eggs are one of the most common allergies in babies and young children, around 70% of children with an egg allergy will grow out of it by the time they reach the age of 16 (1).
Your allergist may recommend an “egg ladder” to build up your child’s tolerance to eggs through very slow, gradual, and consistent exposures. If your baby has an egg allergy, speak to your pediatrician about treatment options.
Can babies react to eggs after multiple exposures with no reaction?
Yes.
This is why it’s important that babies be exposed to eggs multiple times before being able to rule it out as an allergy. A reaction may not occur until the second or subsequent time eggs are offered.
However, if your baby doesn’t ingest much egg the first couple of times, they may not have truly been exposed to enough proteins to determine if they’re allergic or not. Therefore, a reaction could occur after multiple exposures once they ingest enough egg to trigger a reaction.
That said, anyone can develop an allergy at any point, even to a food you’ve eaten safely in the past. This is why introducing priority allergens like eggs early on when starting solids and keeping them in the diet regularly is so important to help reduce the risk of an allergy developing later on in life.
Can you prevent allergic reactions through diet?
Most allergies can’t be prevented completely, but there are a few evidence-based practices that may be helpful in reducing the risk of your baby developing an allergic reaction (19,39).

Easy egg salad recipe for baby led weaning
Equipment
- 1 small pot
Ingredients
- 2 eggs
- 1 ⅓ tbsp mayonnaise
- ½ tsp dried dill
- 1 tsp dried chives (or 1 tbsp fresh chives, finely chopped)
- Black pepper (to taste)
- Toast or rice rusks (optional)
Instructions
- Bring a pot of water to a boil. Once boiling, reduce the heat slightly and add the eggs. Cook for 10 minutes or until fully cooked. Once the eggs are well done, add them to a bowl of ice water. Once they're cool enough to handle, peel and chop or mash.
- In a bowl, combine the mashed eggs, mayonnaise, dill, chives, and pepper.
- Serve to your baby as is in a bowl with a pre-loaded spoon or let them dig in with their hands! Alternatively, spread some egg salad onto a lightly toasted piece of bread (cut into strips or bite-size pieces) or a rice rusk for your baby to self-feed.
Notes
Pin this for later!

References
- American College of Allergy, Asthma, & Immunology. Egg. Retrieved from: https://acaai.org/allergies/allergic-conditions/food/egg/
- Pratico, A. D., Mistrello, G., Rosa, M. L., Guidice, M. M., & Marseglia, G. (2014). Immunotherapy: a new horizon for egg allergy? Expert Review of Clinical Immunology, 10 (5). https://doi.org/10.1586/1744666X.2014.901887
- Djossi. S. K., Khedr, A., Neupane, B., Proskuriakova, E., Jada, K., & Mostafa, J. A. (2022). Food allergy prevention: Early versus late introduction of food allergens in children. Cereus. DOI: 10.7759/cureus.21046
- American College of Asthma, Allergy, & Immunology. (2021). Increased frequency of eating eggs in infancy associated with decreased egg allergy later on. https://acaai.org/news/increased-frequency-of-eating-eggs-in-infancy-associated-with-decreased-egg-allergy-later-on/
- Royal, C., & Gray, C. (2020). Allergy prevention: An overview of current evidence. Yale Journal of Biology and Medicine, 93(5), 689-698. https://pmc.ncbi.nlm.nih.gov/articles/PMC7757062/
- Fleischer, D. M., Chan, E. S., Venter, C., Spergel, J. M., Abrams, E. M., Stukus, D., Groetch, M., Shaker, M., & Greenhawt, M. (2021). A Consensus Approach to the Primary Prevention of Food Allergy Through Nutrition: Guidance from the American Academy of Allergy, Asthma, and Immunology; American College of Allergy, Asthma, and Immunology; and the Canadian Society for Allergy and Clinical Immunology. The Journal of Allergy and Clinical Immunology In Practice, 9(1), 22-43. https://doi.org/10.1016/j.jaip.2020.11.002
- Yakaboski, E., Robinson, L. B., Arroyo, A., Espinola, J. A., Geller, R. J., Sullivan, A. F., Rudders, S. A., & Camargo Jr, C. A. (2021). Early introduction of food allergens and risk of developing food allergy. Nutrients, 13(7), 2318. doi: 10.3390/nu13072318
- American Academy of Allergy, Asthma & Immunology. Atopy Defined. https://www.aaaai.org/tools-for-the-public/allergy,-asthma-immunology-glossary/atopy-defined
- Cukrowska, B. (2018). Microbial and Nutritional Programming—The Importance of the Microbiome and Early Exposure to Potential Food Allergens in the Development of Allergies. Nutrients, 10(10), 1541. https://doi.org/10.3390/nu10101541
- Lv, Y., Chen, L., Fang, H., & Hu, Y. (2024). Associations between diet diversity during infancy and atopic disease in later life: Systematic review. Journal of Allergy and Clinical Immunology: Global, 3(2), 100221. doi: 10.1016/j.jacig.2024.100221
- Caffarelli, C., Giannetti, A., Rossi, A., & Ricci, G. (2022). Egg allergy in children and weaning diet. Nutrient, 14(8), 1540. doi: 10.3390/nu14081540
- Food Allergy Awareness. Egg. https://www.foodallergyawareness.org/food-allergy-and-anaphylaxis/food-allergens/egg/
- Dang, T. D., Peters, R. L., Koplin, J. J., Dharmage, S. C., Gurrin, L. C., Ponsonby, A. L., Martino, D. J., Neeland, M., Tang, M. L. K., Allen, K. J., & HealthNuts study (2019). Egg allergen specific IgE diversity predicts resolution of egg allergy in the population cohort HealthNuts. Allergy, 74(2), 318–326. https://doi.org/10.1111/all.13572
- American College of Allergy, Asthma and Immunology. (2018). Anaphylaxis. https://acaai.org/allergies/symptoms/anaphylaxis/
- Waserman, S., Bégin, P., & Watson, W. (2018). IgE-mediated food allergy. Allergy, asthma, and clinical immunology: official journal of the Canadian Society of Allergy and Clinical Immunology, 14( 2), 55. https://doi.org/10.1186/s13223-018-0284-3
- Cox, L. S., Sanchez-Borges, M., & Lockey, R. F. (2017). World Allergy Organization Systemic Allergic Reaction Grading System: Is a Modification Needed?. The journal of allergy and clinical immunology. In practice, 5(1), 58–62.e5. https://doi.org/10.1016/j.jaip.2016.11.009
- Waserman, S., Bégin, P., & Watson, W. (2018). IgE-mediated food allergy. Allergy, asthma, and clinical immunology: official journal of the Canadian Society of Allergy and Clinical Immunology, 14( 2), 55. https://doi.org/10.1186/s13223-018-0284-3
- Mayo Clinic. Egg allergy. https://www.mayoclinic.org/diseases-conditions/egg-allergy/symptoms-causes/syc-20372115
- Seattle Children’s. Food Allergy. https://www.seattlechildrens.org/conditions/a-z/food-allerg
- BC Centre for Disease Control. Communicably Disease Control Manual. Chapter 2: Immunization: Part 3 – Management of Anaphylaxis in a Non-Hospital Setting. http://www.bccdc.ca/resource-gallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/Epid/CD%20Manual/Chapter%202%20-%20Imms/Part_3_Anaphylaxis.pdf
- Frontier Allergy Asthma & Immunology. How Long Does a Food Allergy Reaction Last? Retrieved from: https://www.frontierallergist.com/how-long-does-a-food-allergy-reaction-last/
- Australasian Society of Clinical Immunology and Allergy. Food Protein-Induced Enterocolitis Syndrome (FPIES). https://www.allergy.org.au/patients/food-other-adverse-reactions/food-protein-induced-enterocolitis-syndrome-fpies
- Food Allergy Canada. Food Protein-Induced Enterocolitis Syndrome (FPIES). Retrieved from: https://www.foodallergycanada.ca/food-allergy-basics/related-conditions/food-protein-induced-enterocolitis-syndrome-fpies/
- Weinberger, T., Feuille, E., Thompson, C., & Nowak-Wegrzyn, A. (2016). Chronic food protein-induced enterocolitis syndrome. Annals of Allergy, Asthma & Immunology, 117(3), 227-233. https://www.annallergy.org/article/s1081-1206(16)30042-4/fulltext
- Nowak-Węgrzyn, A., Jarocka-Cyrta, E., & Moschione Castro, A. (2017). Food Protein-Induced Enterocolitis Syndrome. Journal of investigational allergology & clinical immunology, 27(1), 1–18. https://doi.org/10.18176/jiaci.0135
- North West Paediatric Allergy Network. What is FPIES? https://allergynorthwest.nhs.uk/home-patient/managing-allergies/patient-leaflets/fpies/
- Children’s Hospital of Philadelphia. Food protein-induced enterocolitis syndrome (FPIES). https://www.chop.edu/conditions-diseases/food-protein-induced-enterocolitis-syndrome-fpies
- Paulsen, E., Christensen, L.P., & Andersen, K.E. (2012). Tomato contact dermatitis. Contact Dermatitis, 67: 321-327. https://doi.org/10.1111/j.1600-0536.2012.02138.x
- Kelava, N., Lugović-Mihić, L., Duvancić, T., Romić, R., & Situm, M. (2014). Oral allergy syndrome–the need of a multidisciplinary approach. Acta clinica Croatica, 53(2), 210–219.
- Brown S. J. (2016). Atopic eczema. Clinical medicine (London, England), 16(1), 66–69. https://doi.org/10.7861/clinmedicine.16-1-66
- American College of Allergy, Asthma & Immunology. (2023). Eczema. https://acaai.org/allergies/allergic-conditions/skin-allergy/eczema/
- Health Link BC. Eczema and food allergy in babies and young children. Retrieved from: https://www.healthlinkbc.ca/sites/default/files/healthyeating/pdf/ds_050.pdf
- Prevent Food Allergies. Food Allergic Reaction v. Eczema Flare-Up: Which One Is My Child Having? Retrieved from: https://www.preventallergies.org/blog/food-allergy-vs-eczema-flare-up
- Kids Feeding Team. Egg allergy. Retrieved from: https://www.kidsfeedingteam.co.uk/what-we-treat/allergies-and-intolerances/egg-allergy/
- American College of Asthma, Allergy, & Immunology. (2019). Egg. https://acaai.org/allergies/allergic-conditions/food/egg/
- Chomyn, A., Chan, E. S., Yeung, J., Vander Leek, T. K., Williams, B. A., Soller, L., Abrams, E. M., Mak, R., & Wong, T. (2021). Canadian food ladders for dietary advancement in children with IgE-mediated allergy to milk and/or egg. Allergy, asthma, and clinical immunology : official journal of the Canadian Society of Allergy and Clinical Immunology, 17(1), 83. https://doi.org/10.1186/s13223-021-00583-w
- St. Joseph’s Healthcare. Egg allergy. Retrieved from: https://www.stjoes.ca/patients-visitors/patient-education/a-e/PD%204790%20Egg%20Allergy%20FIRH.pdf
- Food Allergy Canada. Egg. https://foodallergycanada.ca/allergies/egg/#:~:text=Albumin/Albumen,Vitellin
- Zoi, K., Papadopoulou, E., Panteris, E., Papadopoulou, S., Skordou, A., Karamaliki, M., & Diamanti, E. (2023). The effect of breastfeeding on food allergies in newborns and infants. Children. 10(6), 1046. doi: 10.3390/children10061046

Jillian Smith, RD
Registered Dietitian at My Little Eater Inc., and dog-mom to River. Jillian works behind the scenes answering nutrition questions and supporting parents of babies and toddlers to feed their little ones with confidence.
Click below to book a counselling session with Jill today!

Jillian Smith, RD
Registered Dietitian at My Little Eater Inc., and dog-mom to River. Jillian works behind the scenes answering nutrition questions and supporting parents of babies and toddlers to feed their little ones with confidence.
Click below to book a counselling session with Jill today!






3 Comments
When the Witcher anime application launched in 2025, it quickly captured attention and sparked widespread interest in the anime community, becoming especially popular in Arab regions.
A lot of people love the way streaming anime at witcher app and became stuck to it.
I like your way of explaining. Thanks